Understanding Shoulder Dislocations: Causes, Treatments, and Recovery Options from a Sports Medicine Perspective
Shoulder Dislocations: A Comprehensive Guide for Athletes and Active Individuals
Shoulder dislocations are among the most common traumatic injuries seen in sports medicine, especially in contact and overhead sports such as football, wrestling, basketball, and volleyball. If you’ve experienced a shoulder dislocation, understanding your treatment options — both conservative and operative — is critical for optimal recovery and return to activity.
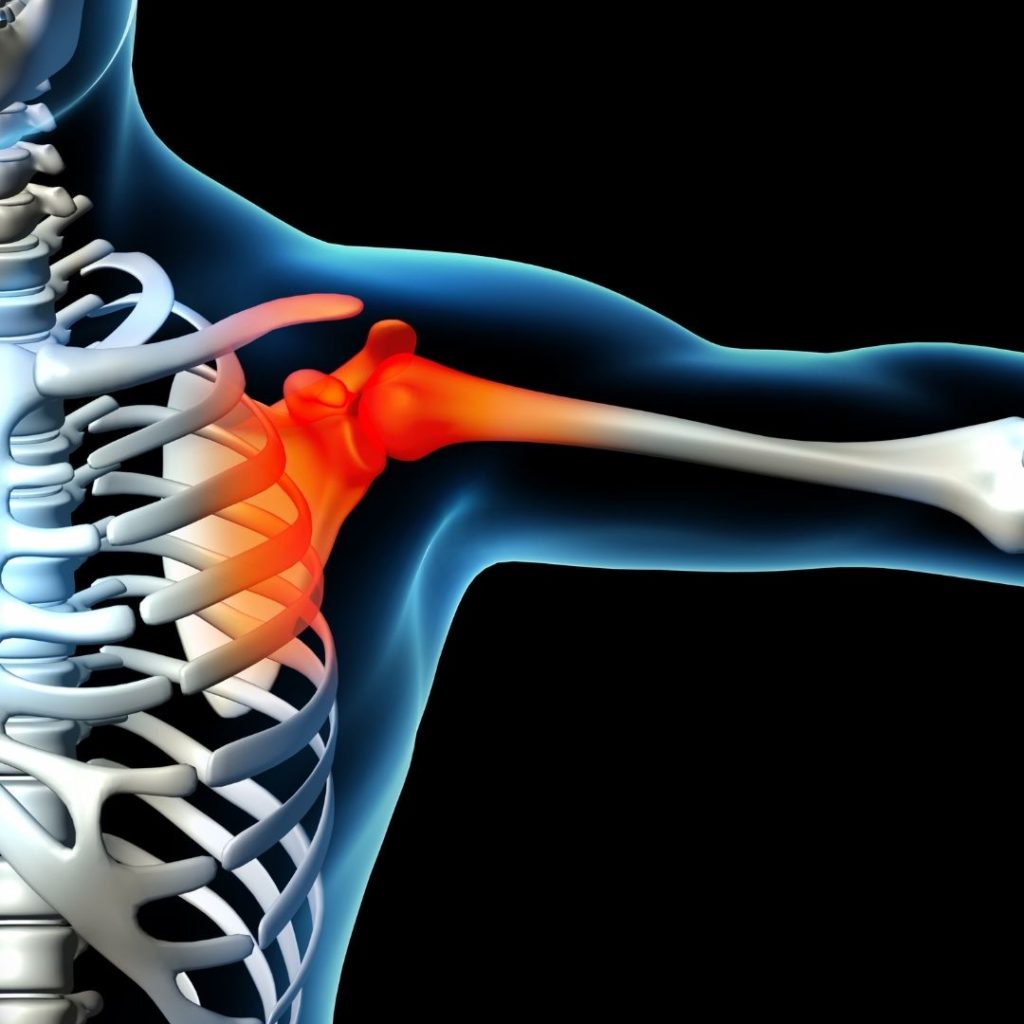
What Is a Shoulder Dislocation?
A shoulder dislocation occurs when the head of the humerus (upper arm bone) is forcibly displaced from the glenoid (socket of the shoulder blade). Due to the shoulder’s wide range of motion and relatively shallow socket, it is particularly prone to instability.
There are three types of shoulder dislocations:
- Anterior dislocation (most common): The humeral head moves forward out of the socket.
- Posterior dislocation: Less common, often caused by seizures or electrical shock.
- Inferior dislocation: Rare and usually associated with significant trauma.
Causes and Risk Factors
- Direct trauma or fall on an outstretched arm
- Sudden, forceful overhead movements
- Weakness or laxity in shoulder ligaments
- Previous history of shoulder instability
Athletes under 25 years old are at the highest risk of recurrence, especially after their first dislocation.
Symptoms of a Shoulder Dislocation
- Sudden, intense shoulder pain
- Visible deformity or asymmetry
- Inability to move the shoulder
- Swelling, bruising, and numbness
Immediate medical evaluation and imaging (X-ray or MRI) are crucial to confirm the diagnosis and assess for associated injuries such as labral tears or bone damage.
Conservative (Non-Surgical) Treatment Options
Conservative treatment is typically recommended after a first-time dislocation in patients without significant bone or soft tissue injury.
1. Closed Reduction
A trained medical professional will gently maneuver the shoulder back into place. This should always be done under appropriate sedation and imaging guidance to avoid complications.
2. Immobilization
The arm is usually placed in a sling for 1–3 weeks to allow soft tissue healing. Recent evidence suggests early motion may be beneficial, especially in older patients.
3. Physical Therapy
Rehabilitation focuses on restoring:
- Range of motion
- Strength of the rotator cuff and scapular stabilizers
- Proprioception and neuromuscular control
Return to sports is generally expected within 6–12 weeks, depending on sport demands and individual recovery.
Operative Treatment: When Surgery Is Necessary
Surgical intervention is often recommended for:
- Young athletes with high recurrence risk
- Repeated dislocations
- Presence of bony lesions (Bankart or Hill-Sachs lesions)
- Failure of conservative management
Common Surgical Procedures
- Arthroscopic Bankart Repair
- Reattaches torn labrum and tightens the capsule.
- Minimally invasive with excellent outcomes in active individuals.
- Latarjet Procedure
- Transfers bone and tendon to the front of the shoulder socket.
- Preferred for patients with significant bone loss or contact athletes.
- Remplissage Technique
- Addresses Hill-Sachs lesions to prevent engagement and re-dislocation.
- Often performed in combination with Bankart repair.
Post-Operative Recovery and Rehabilitation
Recovery timelines vary but generally follow this structure:
- Weeks 0–6: Sling immobilization, passive motion exercises
- Weeks 6–12: Active motion and strengthening
- Months 3–6: Sport-specific training
- 6+ Months: Return to full contact sports
Surgical success rates are high, with over 90% of patients returning to previous levels of activity.
Preventing Future Shoulder Dislocations
- Strengthening rotator cuff and scapular muscles
- Improving flexibility and posture
- Avoiding risky overhead movements in early rehab
- Wearing protective gear in contact sports
Athletes should work with orthopedic specialists and physical therapists to reduce the risk of recurrence and ensure safe return to play.
Final Thoughts
Shoulder dislocations are treatable with both conservative and surgical approaches. Early diagnosis, individualized treatment planning, and structured rehabilitation are key to a full recovery and minimizing the risk of re-injury. Whether you’re a professional athlete or a weekend warrior, consult with an orthopedic sports medicine specialist to determine the best path forward.