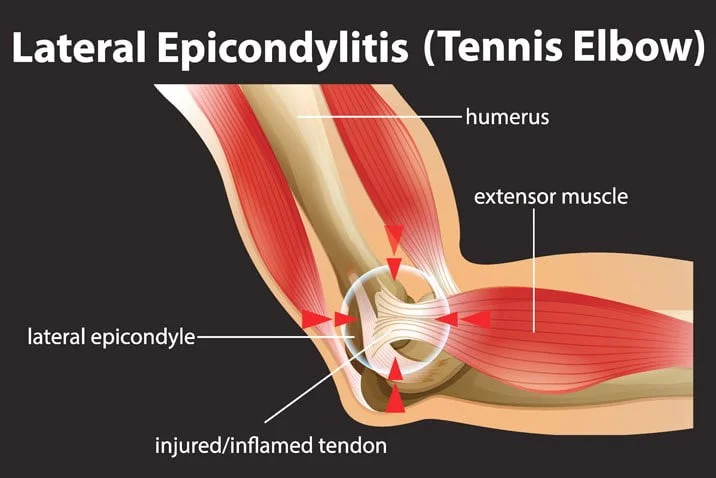
Tennis Elbow (Lateral Epicondylitis): Causes, Symptoms, and Treatment Options (Including PRP)
What is Tennis Elbow (Lateral Epicondylitis)?
Tennis elbow, medically known as lateral epicondylitis, is a painful condition caused by overuse or degeneration of the extensor tendons that attach to the lateral epicondyle — the bony bump on the outside of the elbow. The condition ranges from tendonitis (inflammation) to tendinosis (degenerative changes and microtears) and can cause weakness, pain with gripping, and difficulty with wrist extension. NCBI+1
Causes — Why Does Tennis Elbow Happen?
Tennis elbow results from repetitive loading of the wrist extensor tendons. Common causes include:
- Repetitive wrist extension and gripping — frequent, forceful wrist and finger actions create microtrauma to the tendon. NCBI
- Racquet sports — tennis, squash, racquetball, badminton, and paddle sports are classic causes (incorrect stroke mechanics and repetitive backhand/racquet motions are typical triggers). Note: many people who get “tennis elbow” are not tennis players, but racquet sports are an established risk factor. NCBI+1
- Other sports and activities — throwing sports, weightlifting, gymnastics, and occupations with repetitive wrist/finger use (plumbing, painting, carpentry, computer work). Hopkins Medicine
- Age and tendon degeneration — peak incidence is typically between ages ~30–50 due to progressive tendon wear. OrthoInfo
Symptoms & When to See a Doctor
Typical symptoms include:
- Pain or tenderness on the outside (lateral) elbow.
- Pain aggravated by gripping, lifting, shaking hands, or turning a wrench.
- Weakness in grip or wrist extension.
- Symptoms often develop gradually but can follow an increase in activity or an awkward motion.
See a clinician if pain limits daily activities, lasts more than a few weeks despite home care, or you suspect a tendon rupture (sudden sharp pain, palpable gap, marked weakness).
Diagnosis
Diagnosis is usually clinical — history and exam maneuvers (like resisted wrist extension and the “middle finger test”). Imaging (ultrasound or MRI) is reserved for atypical cases, persistent symptoms, or to evaluate tendon tears. OrthoInfo
Conservative (First-line) Treatment Options
Most cases respond to conservative management over weeks to months:
- Activity modification & relative rest
- Avoid or modify the repetitive motion that provoked symptoms (change grips, reduce practice time, use two-handed backhand where applicable for racquet players). OrthoInfo
- Analgesics & anti-inflammatories
- Short-term NSAIDs for pain (oral or topical) as needed.
- Physical therapy (PT)
- Eccentric strengthening of wrist extensors (e.g., eccentric wrist drops), progressive strengthening, flexibility, and manual therapy. PT focused on eccentric loading has good evidence and is a cornerstone of rehab. OrthoInfo
- Bracing / orthosis
- Counterforce straps or wrist splints can reduce tendon load during activity.
- Ice and soft tissue care
- Short periods of ice for symptomatic relief, plus cross-friction massage and scar/tissue mobilization when appropriate.
- Extracorporeal shockwave therapy (ESWT) & other modalities
- ESWT sometimes used for chronic tendinopathy with variable outcomes in trials.
- Corticosteroid injections
- Often give rapid short-term pain relief but may have inferior long-term outcomes vs other options; repeated steroid injections are not typically recommended because they can weaken tendons and lead to recurrence. (See PRP comparison below.) PubMed
Platelet-Rich Plasma (PRP) for Tennis Elbow — What the Evidence Says
PRP is an autologous blood product concentrated for platelets and growth factors, injected into the degenerative tendon area to enhance healing.
Bottom line from recent systematic reviews and RCTs:
- Short-term (weeks–2 months): Corticosteroid injections commonly provide faster pain relief than PRP. PubMed
- Long-term (≥3–6 months): PRP often shows better or more durable long-term improvement in pain and function compared with corticosteroids and may outperform other conservative injections for some patients with chronic lateral epicondylitis. Several systematic reviews and meta-analyses support PRP’s superior long-term outcomes, though heterogeneity exists across studies (different PRP preparations, doses, injection techniques, and outcome measures). PubMed+2SAGE Journals+2
Key nuances to consider:
- PRP preparations vary (leukocyte-rich vs leukocyte-poor, platelet concentration, single vs multiple injections) — results can differ accordingly. Several recent reviews call for standardized protocols. ScienceDirect+1
- PRP is usually reserved for chronic or recalcitrant cases that have failed conservative therapy (exercise, bracing, activity modification).
- Cost and access: PRP is commonly not covered by insurance and varies in price.
- Safety: PRP is autologous and generally well tolerated; transient injection site pain and stiffness may occur.
Representative evidence citations: multiple RCTs and meta-analyses conclude: corticosteroids faster short-term relief; PRP yields better long-term functional outcomes and pain relief for many patients with lateral epicondylitis. PubMed+2PubMed+2
When Is Surgery Considered?
Surgery is an option for persistent, disabling lateral epicondylitis that does not improve after 6–12 months of comprehensive conservative care (including PT, bracing, injections as indicated). Surgical options include debridement of degenerated tendon tissue, open or arthroscopic release, and sometimes tendon repair or augmentation. Outcomes are generally good in appropriately selected patients, but recovery and rehab take time. OrthoInfo
Typical Recovery Timelines
- Mild cases with activity modification + PT: weeks to a few months.
- Chronic cases requiring PRP or prolonged rehab: improvements often noted by 3 months and more durable gains by 6–12 months. PubMed
- Post-op recovery: return to full activity usually takes several months depending on procedure and rehab.
Practical Clinical Pathway (example)
- Start with activity modification, bracing, and guided physical therapy (6–12 weeks).
- If inadequate response, consider an injection — discuss risks/benefits of corticosteroid (short-term relief) vs PRP (potentially superior long-term results).
- If symptoms persist despite comprehensive nonoperative care for 6–12 months, refer to orthopedics/hand surgery for surgical discussion.