Patellar Dislocations: Causes, Symptoms, and Treatment Options (Operative & Non-Operative)
Signs and Symptoms of a Dislocated Patella
If you experience a patellar dislocation, you may notice:
- A visibly displaced kneecap
- Intense knee pain
- Swelling and bruising
- Inability to straighten or bear weight on the knee
- A sensation of the knee "giving out"
Some people also report recurring dislocations, a condition known as patellar instability.
Diagnosing a Patellar Dislocation
Diagnosis typically includes:
- Physical examination
- X-rays to assess bone alignment
- MRI scans to evaluate ligament damage (especially to the MPFL – medial patellofemoral ligament)
Non-Operative Treatment for Patellar Dislocations
Most first-time dislocations without significant bone or ligament damage are treated non-surgically.
Key Non-Operative Options Include:
1. Closed Reduction
The dislocated kneecap is gently manipulated back into place by a medical professional.
2. Immobilization
Use of a brace or knee immobilizer for 2–3 weeks to allow soft tissues to heal.
3. Physical Therapy
A targeted rehab program focusing on:
- Strengthening the quadriceps, especially the vastus medialis obliquus (VMO)
- Improving flexibility and knee alignment
- Enhancing proprioception and balance
4. Activity Modification
Avoiding high-impact sports until full recovery is achieved.
When Is Non-Operative Treatment Enough?
- First-time dislocations
- No loose bone fragments
- Mild to moderate ligament damage
- Low risk of recurrence
Operative Treatment for Patellar Dislocations
Surgery may be necessary for:
- Recurrent patellar dislocations
- Severe damage to ligaments (e.g., MPFL tear)
- Bone fragments or osteochondral injuries
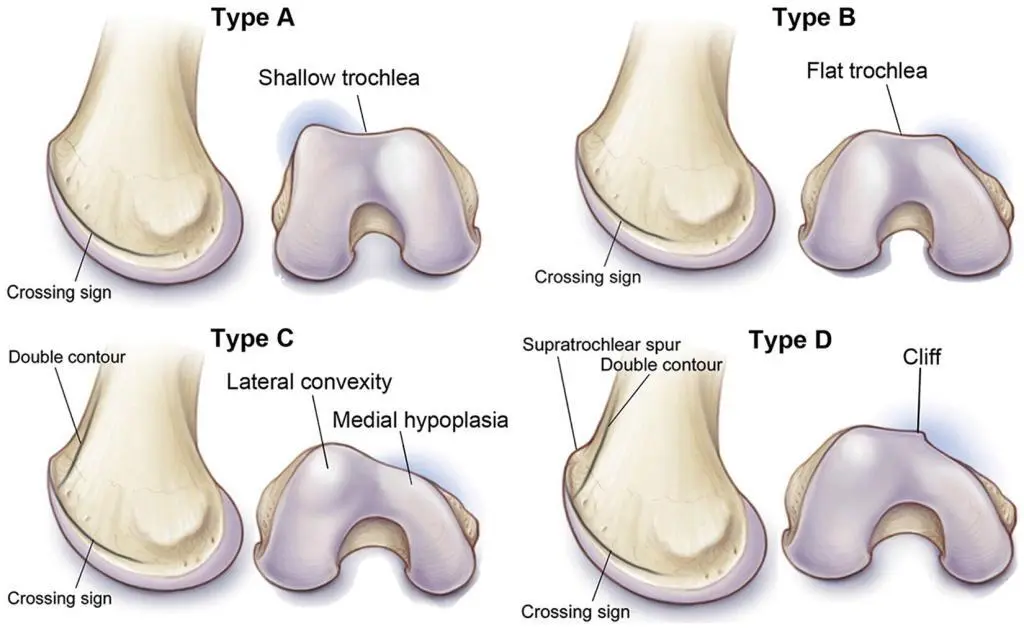
- Anatomical risk factors (e.g., high-riding patella, trochlear dysplasia)
Common Surgical Options Include:
1. MPFL Reconstruction
The medial patellofemoral ligament is rebuilt using a graft, typically from the hamstring tendon, to prevent future dislocations.
2. Tibial Tubercle Osteotomy (TTO)
The bony attachment of the patellar tendon is repositioned to improve patella tracking.
3. Trochleoplasty
A surgical reshaping of the femoral groove to better contain the patella (reserved for complex cases).
4. Arthroscopic Debridement
Removal of loose bodies and repair of cartilage damage.
Recovery After Surgery
- Weight-bearing may be restricted for 2–6 weeks, depending on the procedure.
- Physical therapy begins early to restore range of motion, strength, and stability.
- Return to sports usually occurs within 4–6 months, though high-impact activities may take longer.
Patellar Dislocation FAQs
1. Can I walk after a kneecap dislocation?
Walking may be painful initially, but with proper treatment and bracing, many patients regain mobility quickly.
2. Will it happen again?
Up to 30-40% of first-time dislocators may experience recurrence, especially without rehab or in cases with anatomical abnormalities.
3.Is surgery always necessary?
No. Many people recover fully with non-operative treatment, especially after a first-time injury.
Final Thoughts
Patellar dislocations can be painful and disruptive, but effective treatments exist for both acute injuries and chronic instability. Early diagnosis, appropriate rehab, and surgical intervention (when necessary) offer excellent outcomes for most patients.
Need Help With a Patellar Dislocation?
If you’re dealing with knee instability or have experienced a dislocated kneecap, speak to an orthopedic specialist. Early intervention can reduce your risk of long-term issues and get you back to your active lifestyle safely.