Cartilage Preservation & Joint Restoration Surgery: Understanding MACI & Osteochondral Allograft Procedures
Cartilage Preservation and Joint Restoration Surgery: A Comprehensive Guide
Joint pain and cartilage damage can severely limit mobility and quality of life, especially for athletes and active individuals. Fortunately, cartilage preservation and joint restoration surgery have advanced significantly, offering effective, biologic solutions that delay or prevent the need for joint replacement.
Two cutting-edge procedures—MACI (Matrix-Induced Autologous Chondrocyte Implantation) and osteochondral allograft transplantation—are changing the game for people suffering from cartilage injuries, particularly in the knee joint.
In this article, we’ll explore what these procedures are, who they benefit, and how they promote long-term joint health.
Why Is Cartilage Preservation Important?
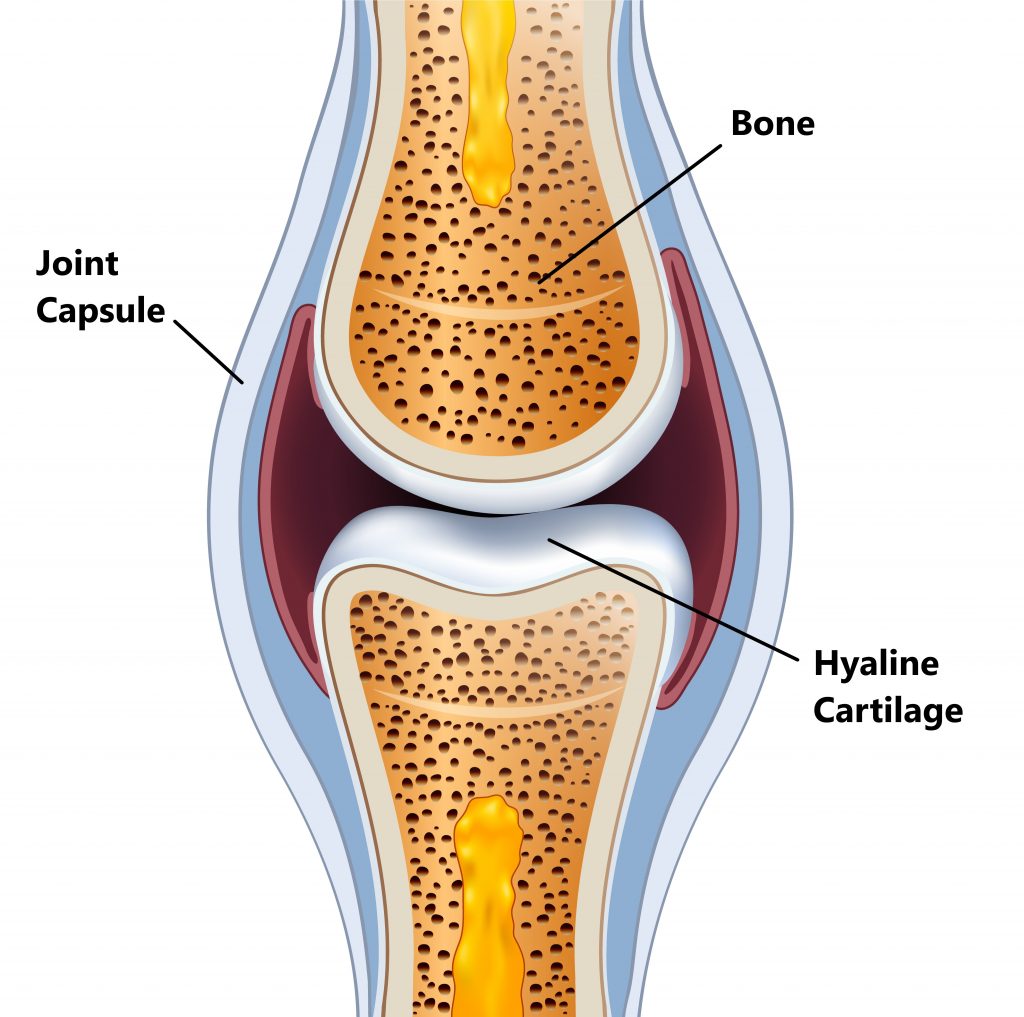
Articular cartilage is the smooth, white tissue covering the ends of bones in joints. It enables low-friction movement and absorbs shock. Unlike other tissues, cartilage has limited capacity for self-healing, making damage from injury or wear-and-tear particularly problematic.
If left untreated, cartilage defects can lead to osteoarthritis, joint instability, and chronic pain. Cartilage restoration procedures aim to repair or replace damaged cartilage before irreversible joint degeneration sets in.
What Is the MACI Procedure?
MACI (Matrix-Induced Autologous Chondrocyte Implantation) is a two-step, FDA-approved procedure used to treat symptomatic cartilage defects of the knee. It is especially effective for active individuals between the ages of 18 and 55.
How MACI Works:
- Cell Harvesting
A small sample of healthy cartilage is arthroscopically removed from the patient’s knee. - Cell Cultivation
The chondrocytes (cartilage cells) are cultured in a lab for several weeks and seeded onto a bioresorbable collagen membrane. - Implantation
The cell-seeded matrix is surgically implanted into the cartilage defect, where it integrates with the surrounding tissue and promotes new cartilage growth.
Benefits of MACI:
- Uses the patient’s own cells (autologous)
- Minimally invasive harvesting process
- Helps restore hyaline-like cartilage
- Reduces pain and improves function
- Delays or prevents knee replacement
What Is an Osteochondral Allograft Transplant?
Osteochondral allograft transplantation is a procedure where a donor cartilage and bone graft is used to repair large or complex cartilage defects, often when other treatments have failed or are not suitable.
How Osteochondral Allografts Work:
- Assessment & Planning
Imaging studies determine the size and location of the cartilage lesion. - Graft Matching
A fresh donor graft that matches the patient's anatomy is selected and shaped to fit the defect. - Surgical Transplantation
The allograft (including cartilage and subchondral bone) is implanted into the damaged area, restoring the joint surface.
Ideal Candidates:
- Younger, active patients with large, full-thickness cartilage defects
- Patients with failed prior cartilage surgery
- Individuals with osteochondritis dissecans or traumatic injuries
Benefits of Osteochondral Allografts:
- Replaces both cartilage and underlying bone
- Can treat larger defects than MACI or microfracture
- Immediate structural support
- No donor site morbidity for the patient
Comparing MACI vs. Osteochondral Allograft Procedures
FeatureMACI ProcedureOsteochondral Allograft TransplantCell SourceAutologous (patient’s own cells)Allogeneic (cadaver donor)Suitable Defect SizeSmall to medium (2–10 cm²)Large (>2 cm², often >4 cm²)Recovery Time6–12 months6–12 monthsIdeal for Younger PatientsYesYesTreats Subchondral Bone?NoYes
Recovery and Rehabilitation
Both MACI and osteochondral allograft procedures require structured rehabilitation, including:
- Physical therapy to restore range of motion and strength
- Non-weight bearing protocols for initial healing
- Gradual return to activity (6–12 months)
- Regular follow-ups and imaging
A successful outcome depends on patient compliance, surgical technique, and individualized rehabilitation plans.
Final Thoughts
Cartilage preservation and joint restoration surgeries like MACI and osteochondral allograft transplantation are transforming orthopedic care. These innovative procedures offer joint-preserving alternatives for patients with cartilage injuries, helping them regain mobility and avoid or delay total joint replacement.
If you're experiencing persistent knee pain or have been diagnosed with a cartilage defect, consult a board-certified orthopedic surgeon who specializes in cartilage restoration. Early intervention can make a significant difference in your long-term joint health.